ROAR Coalition
National Capital Region Organized Against Resistance
Antibiotics Awareness
The National Capital Region Organized Against Resistance urges responsible antibiotic use
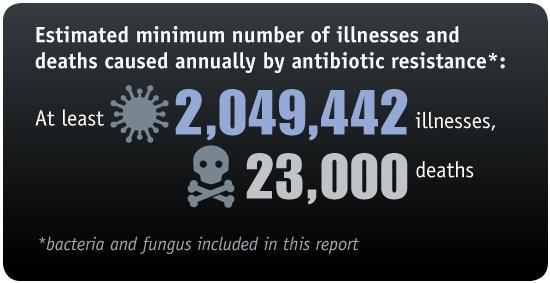
The Challenge
Antimicrobial resistance is one of today’s most pressing public health threats. In an increasingly globalized world, resistant organisms flow continuously across borders and through communities. Individual hospitals cannot address this challenge alone. Even if a facility follows all guidelines for infection control and prescribing, it will still be impacted by patients transferring from other healthcare facilities and moving throughout the community. Every facility must grapple with broader resistance trends, requiring coordinated whole-of-community approaches including learning from each other to adopt and tailor best practices in infection control and antimicrobial stewardship. The Centers for Disease Control and Prevention recently estimated that, over five years, up to 70% fewer patients will get CRE (one of the most serious infections) if facilities coordinate their efforts, as opposed to taking individual action alone.
The National Capital Region is a highly populated area of continual movement where people—and resistance genes—travel easily and often. Visitors from across the country and all over the world arrive and depart daily in large numbers. And, a unique feature of this region is that most area residents commute to and from work across three jurisdictions—Maryland, Virginia, and the District of Columbia. The region is also home to the seat of federal government and many organizations where the global and national policies that address resistance are formulated. These distinctive characteristics provide clear needs and opportunities for a regional approach to: tracking resistance; identifying existing and emerging threats; testing new solutions; and engaging both the health system and the public to help build the awareness needed to galvanize large-scale change.
Who We Are
ROAR is a ground-up effort engaging experts who work day-to-day combatting resistance in their facilities in extending the effort to the broader community, a kind of grassroots population-based laboratory for improving practice that in turn will contribute to the scientific knowledge base and broader policy direction. We are physicians, pharmacists, administrators, infection preventionists, and microbiologists. Our members come from eleven hospitals, all four DC-area medical schools, and two major regional health systems. Member institutions provide both acute and long-term care to a diverse population of all ages and across the socioeconomic spectrum, including minorities, immigrants, military, and veterans. We have established and continue to forge new partnerships with public health and with other health care providers, quality improvement experts, long-term care, outpatient care, and pediatrics. Our current membership roster includes representatives of:
Children’s National Health System
George Washington University Hospital
Howard University Hospital
Inova Fairfax Hospital
Inova Health System
MedStar Georgetown University Hospital
MedStar Health
MedStar Montgomery Medical Center
MedStar Washington Hospital Center
National Institutes of Health Clinical Center
Veterans Administration Medical Center, Washington DC
Virginia Hospital Center
Walter Reed National Military Medical Center
What We Do
We share information, identify common challenges, and collaborate on projects that are priorities for our region in reducing the spread of the most critical multidrug-resistant organisms. We work not only in hospitals but across the continuum of care, and value initiatives that reach patients. We choose initiatives that require cooperation and cannot be accomplished by individual organizations alone. Examples of our initiatives include:
Current
- Developing a community antibiogram that will have numerous potential uses, ranging from regional surveillance to individual facility benchmarking.
- Assessing antibiotic stewardship activities in local long-term care facilities to learn more about what kind of support is needed and be able to provide technical assistance.
- Surveying and sharing information on antibiotic stewardship in acute care—to share promising practices, be able to institute facility-level improvements, and conduct tests that will contribute to the currently limited scientific knowledge base on stewardship interventions.
- Mapping the current state of inter-facility communication on the transfer of patients infected or colonized with multidrug-resistant organisms. The aim is to improve notification systems that will both give providers the timely information needed to treat and protect patients and also contribute to broader regional surveillance.
In Development
- Increasing awareness among providers and the public of the resistance threat and what we can all do to combat it. We believe that a real culture change is needed so that clinicians and patients alike recognize and treat antibiotics as a precious resource.
- Partnering with community care settings outside of acute care hospitals to develop coordinated solutions in patient transfer, communication, and surveillance.